IVUN
INTERNATIONAL VENTILATOR USERS NETWORK
an affiliate of Post-Polio Health International
CONNECTING
VENTILATOR USERS,
HEALTH PROFESSIONALS,
AND INDUSTRY
IVUN
INTERNATIONAL VENTILATOR USERS NETWORK
an affiliate of Post-Polio Health International
CONNECTING
VENTILATOR USERS,
HEALTH PROFESSIONALS,
AND INDUSTRY
VENTILATOR-ASSISTED LIVING
This issue sponsored by:

VOLUME 32, NUMBER 5
OCTOBER 2018
Douglas A. McKim, MD, FCCP, DABSM
This year's Margaret Pfrommer Memorial Lecture in Home-Based Mechanical Ventilation was awarded to Douglas A. McKim, MD, FRCPC, FCCP, DABSM and was presented on October 8th at CHEST 2018 in San Antonio, Texas. Dr. McKim is Professor of Medicine, University of Ottawa and Medical Director, CANVent Respiratory Services and The Ottawa Hospital Sleep Centre in Ottawa, Canada. This was the 18th year the lecture was given at the annual meeting of pulmonologists to educate physicians about home mechanical ventilation..............MORE
Courtesy of CHEST, "When Air Becomes Breath," Audrey King's Margaret Pfrommer Memorial Lecture delivered at CHEST 2017 in Toronto, Canada can now be viewed in its entirety. The text of the lecture was published in Ventilator-Assisted Living last year...............MORE
ADDITIONAL SECTIONS
Networking
Sharing the work of others
Advocacy
Educate, discuss, take action
Recent Relevant Publications
Summaries, links to selected professional, disability, disease journals and newsletters
Educational Opportunities
Conferences and webinars for health professionals and ventilator users
Industry
The business of living with a ventilator
Supported by:
Ventilator-Assisted Living
Vol. 32, No. 5, October 2018
Editor: Brian Tiburzi
Designer: Brian Tiburzi
ISSN 1066-534X
© 2018 Post-Polio Health International.
Permission to reprint must be obtained from Post-Polio Health International (PHI) at info@post-polio.org.
Ventilator users, health professionals, non-profits, company representatives – send comments and updates to info@ventusers.org.
Saving Lives, One Ventilator at a Time…
HMV in 2018… and beyond
The 2018 Margaret Pfrommer Endowed Memorial Lecture in Home-Based Mechanical Ventilation
Douglas A. McKim, MD, FCCP, DABSM
This year's Margaret Pfrommer Memorial Lecture in Home-Based Mechanical Ventilation was awarded to Douglas A. McKim, MD, FRCPC, FCCP, DABSM and was presented on October 8th at CHEST 2018 in San Antonio, Texas. Dr. McKim is Professor of Medicine, University of Ottawa and Medical Director, CANVent Respiratory Services and The Ottawa Hospital Sleep Centre in Ottawa, Canada. This was the 18th year the lecture was given at the annual meeting of pulmonologists to educate physicians about home mechanical ventilation. Established in 1999 by Dr. Allen Goldberg and Dr. Eveline Faure, the lecture honors polio survivor and advocate Margaret Pfrommer from Chicago, Illinois. Pfrommer, a quadriplegic from polio, spent part of her life in a nursing home after her mother’s death. This experience compelled her to become an advocate for herself and for all those with significant disabilities. The purpose of the endowment is to honor an individual who possesses superior knowledge of home mechanical ventilation (HMV) and who promotes the health professional/patient partnership.

Douglas A. McKim, MD
PART 1
It gives me great pleasure to honor the memory of Margaret Pfrommer who was a polio survivor, and much more than an administrative assistant for the Rehabilitation Institute of Chicago. She was a collaborator, helping to design and trial adaptive technologies. She was a fierce advocate for independence and accessibility and helped inform the Americans with Disabilities Act. I also wish to recognize Drs. Eveline Faure and Allen Goldberg for their vision and their untiring support for this presentation as well as the Post-Polio Health International and International Ventilator Users Network for their financial support for the sustainability of this memorial presentation.
I would also like to briefly remember Tony Oppenheimer for his tremendous contributions to the care and well-being of VAIs. He left us too soon. He was a mentor and friend who gave me considerable encouragement early in my career. He was known for his intellectual generosity and as a fierce advocate for patients’ rights.
I live in Ottawa, our nation’s capital, population one million with a very large catchment area, even as far as Iqaluit. The Rideau Canal, a Unesco World Heritage site, was completed in 1832, 20 years after the war of 1812, designed to connect Kingston to Montreal and protect our ships from American cannons in the St. Lawrence River!
The Number Needed to Treat (NNT) is the average number of patients who need to be treated to prevent one additional adverse outcome. One has to treat 125, 67 and 100 individuals respectively in order to prevent one death, one stroke or one MI, in the context of hypertension. 217 would have to undergo low dose lung cancer screening in order to prevent one death, and there is apparently no mortality benefit from statins. In comparison, only eight individuals require treatment with NIV in acute exacerbation of COPD to prevent one death and five to prevent one intubation. What about home ventilation? One in one lives saved?
My interest in noninvasive ventilation was fostered very early. As a second-year medical resident, I helped care for young woman with severe kyphoscoliosis, a vital capacity of less than 1 L, and carry her through respiratory failure using noninvasive volume ventilation.
This was actually my very first publication.
In 1993 I became the Medical Director of the Pulmonary Rehabilitation program and was referred a young woman with severe kyphoscoliosis secondary to a brainstem ependymoma. The resident recognized symptoms of sleep disordered breathing and we successfully diagnosed and treated her nocturnal hypoventilation. We considered this a success, a fait accompli! But was it a success…?

What I was missing was what my first ALS patient’s daughter… and my own daughters were trying to tell me… MIC is the KEY!
I just happened to see an advertisement in Chest for the 5th International Conference on Pulmonary Rehab and Home Ventilation. This is what I was doing. And no one else around me was doing this… I had no colleagues, no mentorship and felt isolated. I met…

By 1997, I had a much better idea how these meetings worked…

I had my first podium presentation presenting the success of entirely outpatient-initiated NIV. I left it, of course, to the real clinician scientists like Manel Lujan (2006), Anita Simmonds (2008) and, most recently, Sheers and Berlowitz (2014) to show that initiating NIV as outpatients is as effective as in-hospital titration, is more acceptable to patients, saves money and may indeed save lives.
Back to 1995. I learned that NIV was indeed important but air stacking was also critical. In order to enhance the legitimacy of air stacking or breath stacking, I coined the term "lung volume recruitment," borrowing from the critical care term ‘alveolar recruitment.’ And we returned to this patient specifically and our population in general to ensure that they were introduced to lung volume recruitment strategies.
This bar graph illustrates the first introduction for this patient to glossopharyngeal breathing. With time both the spontaneous and unassisted peak cough flows increased substantially demonstrating a spontaneous peak cough flow versus assisted peak cough flow difference. This was the first time that I appreciated the possibility of improving respiratory system mechanics as a consequence of LVR.

And this is a video [not available] from our original website, now over 15 years old, demonstrating LVR in a patient with post polio syndrome.
We also identified potentially significant improvements in chest radiography immediately following LVR.
In the view of most patients capable of performing LVR, lung volume recruitment represents freedom… from tracheostomy and represents autonomy and the potential to live independently in the community. It also represents survival - survival without tracheostomy and an opportunity to improve dyspnea and respiratory mechanics, potentially postpone a time when ventilatory support is required and to normalize daytime gas exchange regardless of spontaneous pulmonary function.
We began to explore the effect of LVR in different populations. These are the results of 25 patients with spinal cord injury over an 8 week period of inpatient rehabilitation following acute or chronic injury. There is some increase in spontaneous vital capacity and a marked increase in MIC and assisted peak cough flows with LVR.

We still keep handwritten flow sheets in the CANVent clinic. In this patient with ALS, what this illustrates is a gradual reduction in spontaneous vital capacity with a markedly higher and maintained MIC.
We in fact described this observation at the international symposium of ALS and motor neuron disease in Oakland in 2001, demonstrating the maintenance of MIC and assisted peak cough flows in the face of a marked loss of spontaneous values.

This led to my current view of the world… at least with regard to progressive neuromuscular disease … where, in the face of a progressive loss of vital capacity, with adequate bulbar function, one may be able to maintain for a considerable period of time, a maximum insufflation capacity. This is the same chronology followed by our educational website, I will mention later on.
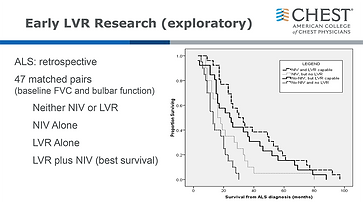
With this in mind, we explored the role of LVR and NIV, in this case in ALS, using pairs of ALS patients matched at baseline for vital capacity and bulbar function and followed with regard to survival, whether receiving no therapy, treatment with noninvasive ventilation alone, LVR alone or the combination of LVR and noninvasive ventilation. One can see that there is a continuum in terms of survival and interestingly, survival with LVR alone actually exceeds that with NIV alone. It is likely that the survival difference has everything to do with maintenance of bulbar function.



Click any image to expand
We began to look at the natural history of LVR in our ALS population. In this illness duration, the number of surviving patients is represented in the dashed black line, falling from just under 100 down to 17 or 18 by the 6th clinic visit. We found that 62% of ALS patients were initially able to perform LVR and that in the surviving patients the MIC remains relatively stable although vital capacity continues to fall and as such the MIC VC difference actually widens, all likely dependent upon maintenance of bulbar function. Similar results are found with spontaneous and assisted peak cough flow.
In 2011 we took these principles and incorporated them in to the first Canadian clinical practice guideline on home mechanical ventilation. We encouraged the regular performance of volume recruitment and airway clearance strategies.
In this case we found that individuals with multiple sclerosis who are able to consistently perform LVR demonstrated a slower reduction in vital capacity and peak cough flow. This is currently being subjected to a two-center randomized controlled trial. The results have not yet been analyzed.

Click image to expand



Click any image to expand
With Dr. Katz, we also found in retrospective analysis that the rate of decline of vital capacity in young people with Duchenne muscular dystrophy can be reduced by the regular performance of LVR, in this cohort, decreasing the rate of loss of vital capacity by almost 90%. This question too is now being assessed in to randomized controlled trials.
Similarly, we have been able to demonstrate that over a period of 8-10 years the MIC and peak cough flow can be maintained at substantially increased values in Duchenne muscular dystrophy with twice daily LVR.
I also recently participated in a study of individuals with respiratory muscle weakness or spinal cord injury, to investigate the acute effects of LVR on respiratory system compliance. In representative illustrations, one can see a marked increase in MIC, respiratory system compliance and a reduction in mean arterial pressure. The latter may be of significance in some individuals prone to hypotension.
Finally, cumulative downloads from NIV can reveal very interesting patterns. This young man with DMD has extreme restriction, a spontaneous VC of only 5% and was introduced to chair-mounted mouthpiece ventilation.
This download of pressure (18/6), rate, tidal volume, % triggered breaths, peak flow and minute ventilation demonstrates a clear increase in tidal volume, flow and minute ventilation as well as a subtle further decrease in the % patient triggered breaths as a consequence of the ability to perform LVR as often as desired with the provision of mouthpiece ventilation. The bilevel parameters are unchanged. This represents a strong suggestion that respiratory system compliance has become more favorable as a result of regular LVR.
Our group has also developed a digital counting device in order to provide objective monitoring of LVR use. This is now being used in 2 prospective randomized controlled trials of LVR.
Here is some preliminary data on adherence from Dr. Katz, 11 Center Canadian study on LVR in children with DMD. The deep blue represents adherence as defined by a minimum of once daily. There is a trend toward improved adherence with diminishing vital capacity.

His data is also being utilized by Nicole Sheers in Melbourne, Australia, where she is also randomizing patients to receive LVR or standard therapy. There appears to be a high degree of agreement between the counts indicated by the digital counter and the diary completed by the participants. Hopefully this digital counter will prove to be useful in further studies of the clinical effects of lung volume recruitment.
Finally, I want to share a unique clinical observation and pose an unanswered question with regard to the combination of pharmacotherapy and LVR.
This 62-year-old radiologist in the inpatient rehabilitation program was noted to have the expected improvements in a restrictive pattern with LVR, increasing his vital capacity by almost 1.4 L (57%).
Although the cause remains unexplained, he developed a pattern of airflow limitation which did not respond to either beta agonists or anticholinergics however interestingly enough, while his MIC response alone was 800 cc, (2.97 up to 3.77 L), with the addition of 4 puffs of Atrovent, this MIC increased by an additional liter to 4.75 L. In other words, the addition of Atrovent with LVR appeared to improve the compliance of the lung.


Click any image to expand
Video Available from Audrey King's 2017 Pfrommer Lecture
Courtesy of CHEST, "When Air Becomes Breath," Audrey King's Margaret Pfrommer Memorial Lecture delivered at CHEST 2017 in Toronto, Canada can now be viewed in its entirety. Text of the lecture may be viewed by clicking the above link.
NETWORKING
Workshop on Walkable and Vibrant Small Towns
Teams from nine small communities (between 2,000 and 18,000) across Alabama gathered in Montevallo for the “ACE Communities Workshop on Walkable and Vibrant Small Towns.” Each team included a planner, a transportation engineer, a public health professional, an elected official, and ask advocate, with several other groups represented, such as educators, health care practitioners, and foundations.

The all-day workshop, facilitated by America Walks’ Ian Thomas, consisted of presentations on best practices in creating walkable communities, a panel discussion featuring staff from state agencies and organizations talking about available resources, a pop-up traffic calming demonstration and series of walkability audits, and structured asset-mapping and goal-setting activities designed to kick-start these teams’ "walkable community planning processes."
Watch a summary video and learn more about tactical urbanism for inclusive community design here.
American Thoracic Society Publishes Flu Prevention Resources
As part of their Patient Education Information Series, the American Thoracic Society has published a factsheet on influenza ahead the flu season. The previous flu season saw close to a million hospitalizations and an estimated 79,000 deaths. Make sure you talk to your health care provider about the best ways to protect yourself. Additional resources can be found on the CDC's flu page.

Webinar Looks at ABLE Successes in the Real World
From the ABLE National Resource Center: For existing ABLE account owners and/or their family members who want to hear concrete real-world strategies and lessons from other ABLE account owners, this is your opportunity to hear from those who are on the front line, pioneering and problem-solving how best to incorporate ABLE into their lives to “achieve a better life experience.”

ADVOCACY
Voting Resources
The U.S. Election Assistance Commission provides timely and useful information to American voters, who deserve accessible, accurate and secure elections. The EAC has a page on their site dedicated to resources for voters with disabilities, including 10 Tips for Voters with Disabilities.
A recent article by eParent detailed some of the barriers that still remain for voters with disabilities, "Obstacles Remain to Exercise of Voting Rights by Individuals with Disabilities."


Another excellent source for information is the American Association of People with Disabilities (AAPD). As part of their REV UP (Register, Educate, Vote, Use your Power) campaign, the AAPD has compiled an extensive list of resources online, including an Issues Guide, Election Accessibility Toolkit and much more.
Supported Decision Making vs. Conservatorship
The Southeast ADA Center recently explored supported decision making and guardianship on their ADA Live! podcast. The episode featured Peter Blanck, PhD, JD and Jonathan Martinis, Esq, JD of the Burton Blatt Institute at Syracuse University, who discussed recent court cases where rights were restored and Supported Decision-Making teams were established.
Under Article 12 of the United Nations Convention on the Rights of Persons with Disabilities (UNCRPD), people with disabilities enjoy legal capacity — the capacity for rights and capacity to act — on an equal basis with others in all aspects of life. Supported Decision-Making (SDM) is a framework that supports this right and helps individuals with disabilities make choices about their own lives with support from a team of people. Supported Decision-Making is an alternative to guardianship.

RECENT RELEVENT
PUBLICATIONS
Competitive Bidding is Here to Stay for Medical Suppliers
Timothy Pigg
“Until recent reforms, winning bidders in competitive-bid areas had to accept the median (composite) price of all bids, which fell below their best-offer bids. This led to price inversions and significant financial pressures and many respiratory therapy providers had no choice but to stop serving the communities they had served for decades. According to a report by the Council for Quality Respiratory Care, there was a sharp 47 percent decrease in the number of home oxygen suppliers in the 10 largest states where the competitive bidding program operates in between 2013 and 2017. Consequently, the patients who require home respiratory therapy and equipment have considerably less choice and access to the life sustaining oxygen they need to maintain their independence and increase their quality of life. This is in fact confirmed by CMS statistics: the percentage of Medicare patients with COPD receiving oxygen therapy has declined 59 percent.”
The Hill. October 30, 2018. Link to article.
Age, Mechanical Ventilation, Disease Severity Influence Hospital Mortality in COPD Patients, Study Says
Diogo Pinto
“Patients were retrospectively identified from ICU databases at the Frankston Hospital in Melbourne, Australia, from January 2005 to June 2016. A total of 305 COPD patients with a mean age of 67.4 years were included in the study.
“Results showed that 77 percent of the patients required noninvasive ventilation, while 38.7 percent required invasive mechanical ventilation (IMV). One-fifth (20.5 percent) of the patients were being managed on home oxygen before the hospital admission.
“Interestingly, a higher in-hospital mortality rate was seen in patients who often required IMV. Also, those who died during hospital admission were more likely to have worse COPD symptoms and to have been on home oxygen.”
COPD News Today. September 18, 2018. Link to article.
Pulmonary circulation disorders predict noninvasive vent failure
Tara Haelle
“COPD patients with pulmonary circulation disorders were more than four times as likely to need invasive ventilation after noninvasive ventilation (NIV) failed for acute exacerbations, found a new study.
“Patients with fluid and electrolyte abnormalities or alcohol abuse also had a greater risk of escalating beyond NIV for exacerbations, according to the findings.”
CHEST Physician. October 8, 2018. Link to article.
Noninvasive ventilation in hypercapnic respiratory failure: from rocking beds to fancy masks
Schreiber A, Fusar Poli B, Bos LD, Nenna R
“Significant developments have occurred in noninvasive ventilation (NIV) over the past two to three decades, such that it is now one of the most evidence-based areas of respiratory medicine. NIV is now part of the standard of care for a variety of conditions such as hypercapnic respiratory failure due to acute exacerbation of chronic obstructive pulmonary disease (COPD) or cardiogenic pulmonary oedema and it has gained prominence in other settings such as in weaning from invasive mechanical ventilation (IMV), in the postoperative period and in palliative care. Indications for the use of NIV continue to expand.”
Breathe. 2018 Sep;14(3):235-237. doi: 10.1183/20734735.018918.
EDUCATIONAL
OPPORTUNITIES
European Repiratory Society livestream
A livestream will be available next month of an ERS course offering, "Noninvasive Ventilation: Advanced." The course, which is being conducted in Milan, Italy, November 22-23, 2018, is meant to provide participants with an overview of the required technical skills in NIV as well as the fields of use and limitations of the different techniques. Find out more.

AARC Congress 2018

AARC’s International Respiratory Convention & Exhibition will take place December 4-7, 2018 at the Mandalay Bay Resort and Convention Center in Las Vegas, Nevada. Find out more and register online.
Canadian Respiratory Conference
The Canadian Thoracic Society will host the 12th Annual Canadian Respiratory Conference in Ottawa, Ontario from April 11-13, 2019. Online registration will open in January 2019.

ATS Conference 2019

The American Thoracic Society will hold their 2019 conference in Dallas Texas, May 17-22. Registration will be available in early December 2018. Click here to complete and submit the form to start your registration.
Focus 2019
Focus 2019 Conference, September 20-21, 2019, Memphis, TN, The Guest House at Graceland, for Respiratory Therapists, Sleep Technologists and Pulmonary Function Technologists. Registration is open.
A second conference will take place in 2019 at the Poughkeepsie Grand Hotel in Poughkeepsie, New York on Wednesday, October 2nd, 2019. This well-established conference will be celebrating its 40th anniversary and is one of the longest continuously running Respiratory Care & Sleep Medicine conferences in the country.
INDUSTRY
DME Competitive Bidding Program Education
ResMed has been working with other industry stakeholders to prepare a comprehensive resource for understanding new competitive bidding program rules that are expected to be finalized in November. The website www.dmecbpeducation.com is a collaboration between leading industry trade organizations to help prepare Durable Medical Equipment Suppliers for Medicare's next round of the Durable Medical Equipment, Prosthetics, Orthotics and Supplies (DMEPOS) competitive bidding program by compiling publicly available information in one place. At present, there is very little information on the site. Once the final rule has been published, information will be added to the various sections.

